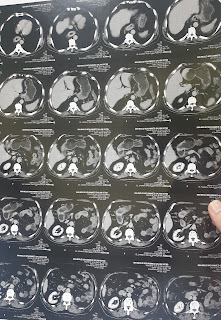
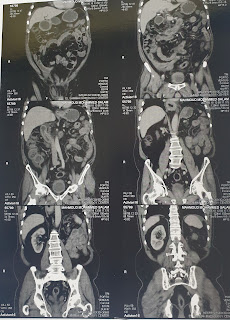
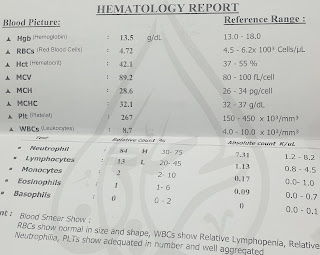
A 63-year-old man presented with chronic abdominal pain of 2 months duration and was referred for upper GI endoscopy. The patient's pain is diffuse and persistent and has not been referred to other sites with a severity of 7/10, according to the pain scale. The pain is associated with nausea and anorexia and prevents the patient from eating. The patient's pain is not relieved with simple analgesics and antispasmodics. A computed tomography scan revealed mural thickening of the gastric pylorus and small bowel loops measuring 13 mm in maximum thickness with minimal ascites. The history is remarkable for an attack of shoulder and back pain 20 years ago that was treated with nonsteroidal anti-inflammatory drugs that affected the stomach and led to epigastric pain managed with PPIs. Clinical examination is remarkable for abdominal tenderness and generalized skin #vitiligo. The patient underwent an upper digestive #endoscopy. The scope revealed inflammation in the pyloric region, duodenum, and lower esophagus. Also, there is a hiatus hernia, gastropathy, and mucosal erythematous mottling with prominent veins in the fundus. Multiple biopsies were taken for histopathology. Pathological examination showed:
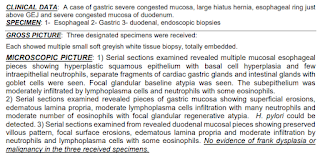
1-reflux esophagitis and separate fragments of gastric cardia-type mucosa with focal
intestinal metaplasia, negative for dysplasia.
Comment: if the biopsy is taken from the tubular esophagus and the mucosal irregularity
extends to at least 1 cm above the top of gastric folds, this represents Barrett's
esophagus. If the biopsy is taken from the cardia, this means intestinal
metaplasia of the gastric cardia.
2-chronic gastritis, with moderate intensity, marked activity, associated with h.
pylori, with focal reparative atypia for follow-up.
3- moderate active chronic non-specific duodenitis with surface erosions.
Questions:
1- Is this diagnosis sufficient to begin treatment, or are more investigations needed?
2- What else to reach a diagnosis?
3-is there a relationship between the previous attack of arthritis and the vitiligo and the GIT symptoms?


Comments