A 78-year-old man presented with dyspepsia, dysphagia, and vomiting and was admitted to the endoscopy unit. The patient has had a history of dyspepsia and dysphagia over the past three months with a slowly progressive course of symptoms. The patient underwent upper digestive endoscopy. The scope revealed fluid and food in the upper stomach and a sizeable annular mass in the body and pyloric region involving the lesser and greater curvature. The mass also encroached on the pyloric ring. The stomach is functionally stenosed (improper motility) but opened structurally. Multiple biopsies were taken for pathological examination. What are your thoughts about this case?
The answer to the case:
Pathology reveals atypical lymphoid proliferation suggestive of MALT lymphoma.
 |
| H&E |
 |
| cd20 |
 |
| ki67 |
 |
| CK |
BCL6
 |
| CD10 |
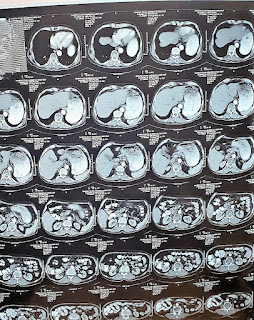 |
| computed tomography showing gastric outlet obstruction after completion of chemotherapy |
 |
BCL2Updates regarding the current casehttps://youtu.be/IHkaDyzsQoI The patient received an entire course of chemotherapy. #Reevaluation after completion of therapy revealed that computed tomography and #PET scans are completely free. Clinically the patient lost weight, and there was repeated vomiting and dyspepsia. We advise an upper GI endoscopy despite the unremarkable radiological studies. The patient underwent a digestive endoscopy after 72 hours of fasting. The scope revealed a massive amount of food and fluids. The patient underwent another upper digestive endoscopy 2 days later, which showed a small number of fluids and food and a sizeable gastric ulcer https://youtu.be/19CPGKhz_ls. The scope can't pass into the duodenum. We ordered a computed tomography of the abdomen with stomach protocol. The tomography revealed complete pyloric obstruction despite no abdominal masses. Also, ultrasonography shows retained food and fluid in the stomach: https://youtu.be/3gChj2uFJ2M QUESTIONS1- your suggestions2- why do we not consider the scope a reevaluation prerequisite when treating GI malignancies? |





Comments